Medical weight management provides structured approaches for patients struggling with excess weight. Healthcare professionals now access advanced treatments beyond traditional diet and exercise recommendations. Keep reading to find out more.
Advanced Weight Management Technologies
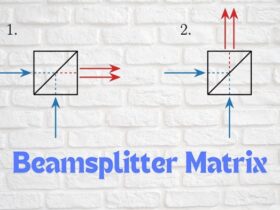
Modern medical weight management incorporates sophisticated technologies for assessment and treatment. Digital health platforms enable continuous patient monitoring between clinic visits. Body composition analysers provide detailed measurements of fat, muscle, and water percentages, allowing for more precise treatment planning than traditional BMI calculations alone.
Metabolic testing equipment helps determine individual caloric needs with greater accuracy. This technology measures resting metabolic rate, giving practitioners data to create personalised nutrition plans. Remote monitoring devices track patient activity levels, sleep patterns, and even eating behaviours, providing valuable insights for treatment adjustments.
For patients requiring additional support, seeking weight loss support through qualified healthcare providers gives access to prescription medications alongside technological interventions. Oxford Online Pharmacy offers consultation services where healthcare professionals determine suitable medical options based on comprehensive patient assessments.
These technological advances allow healthcare providers to create more personalised treatment plans and monitor patient progress with greater precision than ever before. The integration of these tools into clinical practice represents a significant step forward in medical weight management.
Clinical Application of Weight Loss Treatments
Implementing weight loss medications requires systematic clinical protocols. Patient selection criteria involve a comprehensive evaluation beyond simple BMI measurements. Practitioners assess weight history, previous intervention attempts, comorbidities, and genetic factors before recommending pharmacological approaches.
Initial clinical assessment includes detailed metabolic panels, cardiovascular screening, and psychological evaluation. Treatment plans typically involve staged interventions, beginning with lifestyle modifications before adding pharmacological support.
Prescription protocols for weight loss medications follow structured guidelines. Starting doses typically remain conservative, with gradual titration based on response and tolerability. Regular monitoring allows for dosage adjustments and assessment of treatment efficacy against established milestones.
Clinical management extends beyond prescription writing. Practitioners must provide concurrent nutritional guidance, physical activity recommendations, and behavioural support.
Treatment duration varies based on individual response and safety considerations. Some medications suit short-term use during intensive weight loss phases, while others support longer-term management for selected patients. Regular reassessment determines when medication tapering or discontinuation becomes appropriate.
Patient Eligibility Determination
Clinical guidelines establish specific criteria for weight loss treatment eligibility. Understanding these parameters helps healthcare providers make appropriate recommendations for individual patients.
Medical history evaluation forms the foundation of eligibility assessment. Cardiovascular conditions, psychiatric disorders, pregnancy status, and medication use can significantly impact treatment options. Comprehensive screening identifies both absolute and relative contraindications for specific interventions.
Current health status assessment includes laboratory testing, physical examination, and functional assessments. These evaluations establish baseline measurements while identifying potential risk factors or contraindications. Body mass index serves as one criterion, with treatments typically recommended for patients with a BMI ≥30 or ≥27 with weight-related comorbidities.
Previous treatment response documentation helps determine appropriate next steps. Patients who demonstrated inadequate response to lifestyle interventions despite good adherence may benefit from pharmacological approaches.
Patient readiness assessment evaluates psychological factors and practical capabilities for treatment adherence. Successful outcomes require a patient’s understanding of treatment requirements and a willingness to participate actively in the comprehensive program.
Treatment Efficacy Assessment
Systematic monitoring helps practitioners evaluate treatment effectiveness and make necessary adjustments. Multiple metrics provide comprehensive insight into patient progress beyond simple weight measurements.
Anthropometric measurements track physical changes throughout treatment. Beyond scale weight, practitioners monitor waist circumference, body composition percentages, and other relevant measurements. These assessments help quantify changes in body fat distribution, particularly visceral fat reduction associated with metabolic improvements.
Metabolic parameter improvements frequently precede significant weight changes. Blood glucose levels, lipid profiles, and inflammatory markers frequently show early positive responses to treatment. These improvements reflect beneficial physiological changes even when weight loss appears modest.
Functional capacity assessments measure practical improvements in daily activities. Simple tests like timed walks, stair climbing capacity, or validated questionnaires document functional gains. These assessments help patients recognise meaningful improvements beyond aesthetic changes.
Quality of life metrics evaluate the treatment’s impact on overall well-being. Validated assessment tools measure changes in energy levels, mood, sleep quality, and social functioning. These measurements capture important treatment benefits that scale weight cannot reflect.
Comorbidity status tracking documents changes in weight-related health conditions. Improvements in blood pressure control, diabetes management, sleep apnea severity, and joint pain provide significant treatment success markers. These changes often motivate continued treatment adherence despite weight loss plateaus.
Weight Management Continuity Protocols
Long-term weight management requires a structured transition from intensive treatment to maintenance strategies. Healthcare providers implement specific protocols to support sustained results.
Medication tapering follows systematic schedules when transitioning from pharmacological support. Gradual dosage reductions allow physiological adaptation while strengthening reliance on established lifestyle changes.
Monitoring frequency adjustments balance continued oversight with patient independence. Treatment transitions typically involve the gradual extension of intervals between clinical assessments.
Support structure transitions help patients maintain progress after completing intensive treatment phases. Referrals to maintenance programs, support groups, or periodic check-ins provide continued accountability. Digital health tools often supplement these structures with automated monitoring and feedback.
Self-monitoring skill development enables patients to recognise and address small changes before significant weight regain occurs. Practitioners teach specific techniques for regular assessment, problem-solving, and appropriate intervention without medical dependence for minor adjustments.

















Leave a Reply